Best Practices
Context of the practice
Many health facilities in Sri Lanka, India, Kenya, Tanzania, Nepal, and Bangladesh have achieved increasing rates of institutional deliveries. However, the proportion of postnatal women leaving the facilities without receiving a contraceptive method remains high.
PPIUCDs are still emerging as a relatively new contraception choice in India, just like rediscovering the languishing innovation. This low use in spite of good knowledge about IUCDs is attributed to the lack of trained providers, poor quality of IUCD services, provider bias against IUCDs, and a lack of awareness and misconceptions about the method among both clients and health care providers. All these issues have to be addressed by appropriate training of the staff in our department, including doctors, nurses, counselors and other health care providers as well as counseling of the patients in the antenatal period.
Special training is required for immediate postplacental insertions and for insertion within the first 2 days.
Total allotted budget : Rs. 60,89,384.36/-Objectives of Practice
The objective of this practice is to address the postpartum contraceptive needs of women by institutionalising the practice of offering immediate postpartum Intrauterine Device services (IUD) at JSS hospital, Mysuru.
This program was started on 1st May 2015, at JSS hospital, Mysuru.
As women delivering in health facilities rarely return for contraceptive services, the immediate postpartum period presents an ideal opportunity to serve these women with a much-needed service. Long-acting reversible contraceptive methods such as the IUD enable a woman to plan her family and space her pregnancies, allowing more time to look after her child. A pregnancy-free interval also provides time for a woman to be more productive, increasing the family and community income. Furthermore, birth spacing helps to improve the health of the mother and her baby. Copper IUDs can be used effectively for over 10 years by women who want to limit or space their pregnancies; they have the lowest rates of discontinuation; are cost effective; and can be provided by mid-level providers after suitable training. The woman does not need to come back to the clinic for new supplies as she would with other types of contraceptives and the device can be removed at any time with an almost immediate return of fertility. As such, this form of long acting reversible contraception can be an attractive option for postpartum women. There is growing evidence that training on the appropriate technique for healthcare providers can reduce the expulsion rate to a low and acceptable level.
Multiple barriers to service provision can be overcome by counselling in the antenatal period as well as immediate postpartum period on family planning and IUCD insertion to women opting for institutional deliveries.
The Practice
One-third of the maternal deaths and 10% of child mortality can be avoided when couples space pregnancies more than 2 years apart. It is in the first postpartum year that Indian women are most susceptible to unwanted pregnancies. Postpartum family planning is the prevention of unintended and closely spaced pregnancies through the first 12 months following childbirth.
Analysis of NHFS 2 data shows that about one-fifth of the births in India are unplanned. Of these, 12% were mistimed and 9% were unwanted births. The main reason for seeking abortions is for spacing births. Although unmet need for contraception existed for all age groups, it was higher in younger women than in older women.
Among other methods, postpartum IUCD is an effective way to tackle this unmet need of contraception. Although any intrauterine device can be used for postpartum contraception, Copper T 380A which is widely available in institutions and private sectors is one of the most cost-effective options available. It comes in regular and safe load varieties. Copper T 380A is highly effective for 12 years though approved for use only for 10 years. It is a non-hormonal IUCD that can be safely used by all women even during breastfeeding. It requires only one time motivation and few follow-ups.
According to the World Health Organization Medical Eligibility Criteria, an IUCD can be inserted in the 48 h postpartum, or after 4 weeks following birth if that window of 48h is missed. According to a 2010 Cochrane review, PPIUCD is a safe and effective contraceptive method. Presently in India only 2% of the current contraceptive users are using interval Copper T for contraception. Because of increased accessibility to medical care during childbirth, PPIUCD can be offered to all women.
In our hospital, counselling is started from the first antenatal visit. Counselling is done to the pregnant woman and her family members regarding the advantages of PPIUCD and its complications
Insertion is done
- immediately after the placental delivery – postplacental
- within first 48 hours after delivery – postpartum
- during caesarean section – intra caesarean
Evidence of Success
The program was started from 1st May 2015. The antenatal women were counselled about PPIUCD. In patients who had queries about the program, repeated counselling was done by audio-visual aids and charts. Unbooked cases were also counselled in the labour ward. PPIUCD was inserted. In the postpartum period, patients were called for follow-up after 6 weeks and thereafter if they had any symptoms like excessive bleeding, pain abdomen or missed cycle.
Total allotted budget : Rs. 60,89,384.36/-
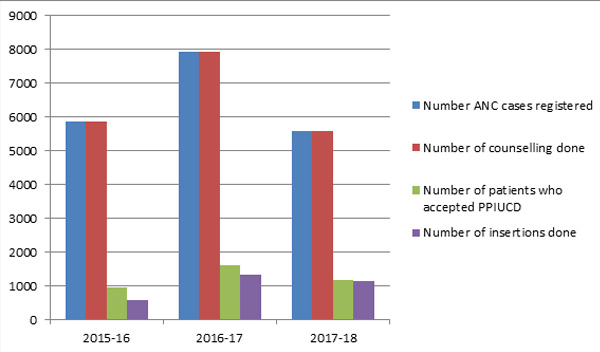
- In the 1st year (2015-16) ANC cases registered - 5870. All of the registered patients were counselled for PPIUCD insertion. The number of patients who were willing for PPIUCD insertion was 961, of which PPIUCD was inserted for 571 patients.
- In the 2nd year (2016-17) ANC cases registered - 7927. All of the registered patients were counselled for PPIUCD insertion. The number of patients who were willing for PPIUCD insertion was 1612, of which PPIUCD was inserted for 1318 patients.
- In the 3rd year (2017-18) ANC cases registered - 5570. All of the registered patients were counselled for PPIUCD insertion. The number of patients who were willing for PPIUCD insertion was 1170, of which PPIUCD was inserted for 1130 patients.
- Due to repeated counselling, there has been a gradual rise in the acceptability for PPIUCD insertion
Problems Encountered and Resources Required
Lack of skilled personnel: To begin with, there were only two master trainers. This was a hindrance for the project due to the unavailability of skilled personnel for round the clock insertion. This was overcome by training more medical and paramedical staff in different phases. The training sessions included lectures, discussions, and hands-on sessions, and pre and post evaluation of the participants. At the end of each session, the participants were evaluated for their skill in insertion technique. This helped raise the number of insertions.
Lack of materials: this was overcome by developing charts, hand-outs, posters, modules and videos showing PPIUCD insertion method to the clients.
Orienting staff (paramedical included) to the benefits and strengths of these services, ensuring high-quality training and post-training followup, and emphasizing quality of services that include infection prevention practices, and training management and monitoring will go a long way in preventing complications.
Strengthened positive counselling at all facility levels by ensuring that all providers, including nurses, are trained in counselling skills is essential. Required counselling materials such as job aids and posters should be made available to all intervention sites. The audio-visual medium can be used to counsel patients. Improved follow-up by establishing a follow-up mechanism and regular monitoring of all clients will boost the programme.
Gallery




